Are you struggling with acne, dermatitis, rosacea, or dry, itchy skin? Have you tried countless topical solutions and creams without success? Read on, as we’re about to dive into a different approach that might just be the answer you’re looking for. Here’s how to achieve healthy skin from the inside out.
Rather watch or listen?
Why Focus on Internal Health for Skin Treatment?
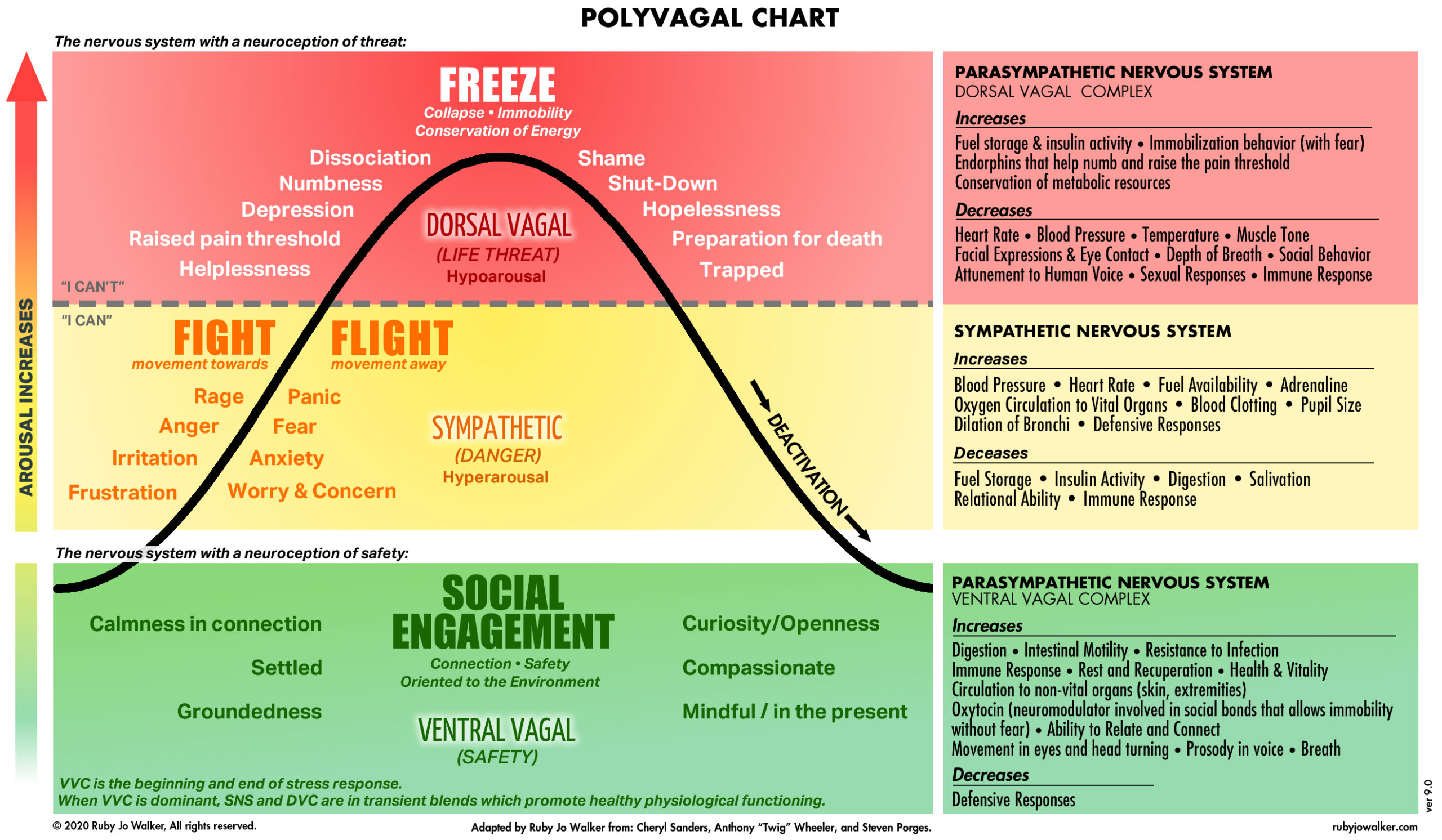
Often, we rely on topical solutions without addressing the root causes of our skin issues. Today, we’ll explore the importance of looking inward to improve skin health. The gut-skin connection, detoxification, and hormonal balance are key factors to consider. Many patients, frustrated with ineffective topical treatments, find success by addressing these internal aspects.
Ways to Improve Your Skin from the Inside
Here are some effective strategies to enhance your skin health from within:
Avoid Processed Foods and Refined Sugars
These can promote inflammation and lead to various skin conditions. Limit their intake to see improvements.
Optimize Protein Intake
Aim for 25 to 30 grams of protein per meal, preferably from hormone-free animal sources. If needed, use supplements like hydrochloric acid and pepsin to aid protein digestion.
Emphasize Omega-3s and Omega-9s
Include fatty fish like salmon, mackerel, and sardines in your diet for Omega-3s. Add almonds and olive oil for Omega-9s. Maintain a balanced ratio of Omega-3s to Omega-6s.
Eat Plenty of Fruits and Vegetables
Aim for 5 to 9 servings a day to boost your intake of antioxidants and polyphenols, which combat oxidative stress.
Stay Hydrated
Drink at least half your body weight in ounces of water daily. Supplement with electrolytes, or add lemon and sea salt to your water to ensure proper hydration.
Avoid Dehydrating Substances
Reduce consumption of alcohol, coffee, certain teas, and caffeine, as these can dehydrate your skin.
Limit Trans Fatty Acids and Mind Your Cooking Methods
Avoid trans fats and be cautious with high-temperature cooking methods like grilling, which can produce harmful compounds that contribute to skin inflammation.
Additional Lifestyle Considerations
Daily Lymph Drainage
Techniques like dry brushing can promote natural detoxification. Check out my other blogs for more on this topic.
Use Safe and Clean Products
The Environmental Working Group Skin Deep database is a great resource to check your products for toxins and allergens.
Optimize Your Sleep
Quality sleep is essential for skin restoration and repair. Poor sleep can accelerate aging and inflammation.
Consult with Professionals
It’s crucial to understand the root causes of your skin issues, which can vary from person to person. Conditions like rosacea, gut dysbiosis, and hormonal imbalances can significantly impact skin health. Consulting with an esthetician and other health professionals can help you develop a tailored skincare routine and address underlying issues.
Final Thoughts
The strategies discussed today are easy to implement and can lead to significant improvements in your skin health. Remember, nutrition and lifestyle changes play a crucial role in achieving healthy skin from the inside out.
If this was helpful, please give it a like, share it, and subscribe to our YouTube channel, the Movement Paradigm, for weekly tips on mindset, nutrition, and movement. Our goal is to help you live your best life, heal, transform, and, more importantly, thrive.
You can always join us in our app, the Movement Paradigm. We have lots of challenges every other month—everything from movement to the nervous system, nutrition, and so on. And we have a great community of people.
You can also reach out to us for an individual appointment for functional medicine or holistic physical therapy. If you really want to get to the root cause, please reach out to us.