Are you experiencing chronic neck pain? Do you feel like you’re always holding tension in your neck, and no matter how many stretches you do, it just does not seem to resolve? Today, we’re going to talk about some root causes of neck pain. Also, of course, some solutions for it.
Rather watch or listen?
4 Neck Pain Causes
1. Breathing and/or airway dysfunction
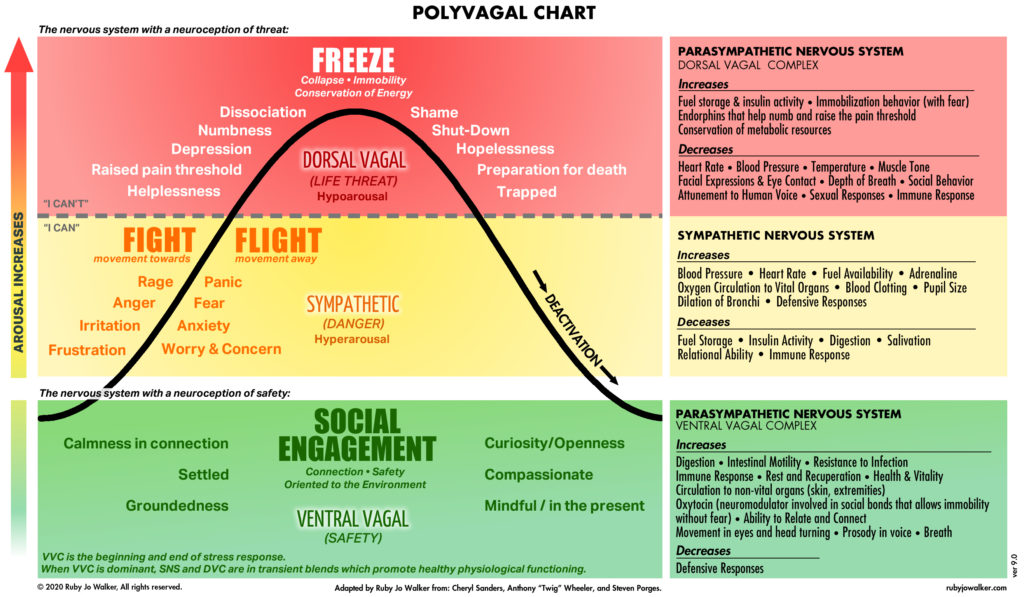
Let’s start with one of the biggest issues, which is some type of breathing and/or airway dysfunction. This means that we can be in a sympathetic state, indicating that we’re in that fight or flight state. This means that we’re going to be breathing from our neck and shoulders.
We breathe 25,000 times a day. So, if every breath is coming from here, you can appreciate how tight this is going to be. We can also have an airway dysfunction, indicating that there could be a deviated septum, a narrow airway, or changes in the jaw. Even poor tongue posture can play a role in exacerbating these issues.
In essence, many things might indicate that there is an airway issue contributing to poor breathing throughout the day and during sleep.
2. Posture
Although there’s no clear link between posture and neck pain, we want to think about any potential compensatory patterns that we have in our body, as they can ultimately lead to compensation in movement and, potentially, pain.
For instance, if you spend long hours at your desk staring at a computer, you might develop certain habits. If you’re always looking at the screen to the left, your muscles and tissues may adapt to that position over time, becoming shorter and possibly causing discomfort.
This doesn’t mean you can’t move your head in different ways, but it’s worth paying attention to regular activities to see if there’s a chance to adjust and put yourself in a better position. Making small changes might help prevent potential pain down the road.
3. Headaches or migraines
If you’re experiencing any ongoing headaches or migraines, this often can be associated with neck pain. But, once again, we want to understand the underlying causes of that. Many times, it can be associated with jaw clenching, which can be correlated with airway dysfunction.
4. Lack of stability or motor control
Neck pain occurs when the neck compensates for a lack of stability or motor control, which we refer to as sequencing, timing, and coordination, somewhere else in the body. A good example of that is our core or abdominal area. It’s a beautiful balance of having the respiratory diaphragm work in synergy with our pelvic diaphragm, and all these muscles need the right coordination to stabilize our spine. This way, we can generate force and move efficiently in everything we do.
If we lack stability in the core, then something in the body has to figure out what to do for that. So often, that can be the neck. For instance, if you are trying to do a core exercise on the ground, and instead of the core really doing what it’s supposed to do, you start to get tension and abnormal tension in your neck. It’s a perfect example of how this could happen.
5 Neck Pain Solutions
So what can you do about it?
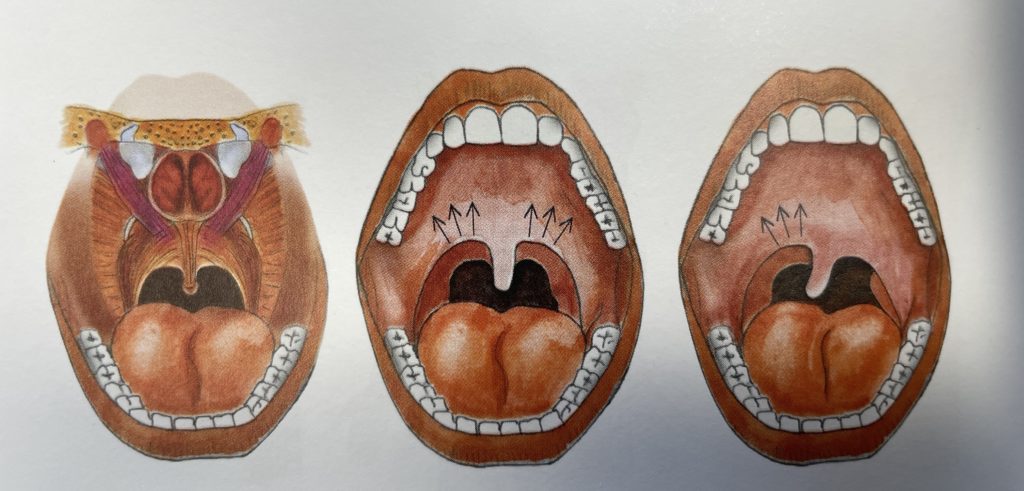
1. Optimize your breathing
Let’s talk about some key points. First, address your tongue position. The resting tongue position should be on the roof of the mouth, gently touching the top teeth. This allows our airway to open so we can get optimal breath. We want to think about breathing in through the nose, and instead of breathing straight back, think about breathing up. As you breathe in, aim for full expansion in the abdomen. Think of it as a 360-degree breath—front, back, and sides of the abdomen. This creates inter-abdominal pressure. As you exhale, the abdomen contracts and the ribs come down.
If you feel like you can work on your breathing and improve it over time, that’s amazing. If it seems challenging to improve, you might need to explore other options to identify if there is indeed some structural airway issue that may need addressing.
2. Stop stretching
Often, when we have neck pain, our instinct is to stretch and stretch. When anything is tight in the body, these muscles are doing exactly what we need at the time—they’re protecting us. So if there’s a lack of stability somewhere else, if breathing is not optimal, then our body is doing what it needs to do to compensate and maintain homeostasis or balance.
We want to be kind to it. If we just take away that compensation, it might have a temporary fix, but it won’t be an ongoing solution. Instead, I love recommending the salamander stretch.
You’ve probably seen this in my other blogs and videos, but it’s worth repeating. This is based on Stanley Rosenberg’s work. Interlace your fingers, bring them behind the back of your head, and relax your arms. Keep your arms down, side bend your upper body and look with your eyes in the opposite direction. Hold this for about 30 seconds. You might experience a sigh, swallow, or yawn—a sign of relaxation. Come back to center, then switch to the other side, eyes in the other direction, holding for 30 seconds. Before and after you perform this exercise, I recommend checking your range of motion. Normally, there is an immediate improvement afterward.
3. Identify any habitual patterns
Is your computer screen over to the left? Can you move it right in front of you? Are you on your phone for hours looking to the right? Just observe these things that you might be doing all day long and consider making some modifications. You don’t need to have perfect posture all day long—I’m not suggesting that. But it might be beneficial to change some of these habits that you’re doing for hours and hours a day.
4. Create stability and strength in the rest of the body
Learn how to build a resilient body. I know that might sound like a lot, but when we think about becoming stronger from the ground up, from our feet up, we can establish a strong connection and have a foundation for stability, strength, and mobility. This way, our neck doesn’t need to compensate all the time. When there’s chronic neck pain, unpacking things such as optimizing breathing, building stability and mobility (for example, in the thoracic spine), and then building strength can truly shift the trajectory of your pain in a lasting way.
5. Identify causes of chronic pain
And last but not least, whenever we have chronic pain, we want to consider a couple of other things. First, is there any systemic inflammation occurring? Are there factors such as certain foods, hormonal imbalances, or chronic stress playing into this systemic inflammatory response, especially when the pain persists? Additionally, we want to distinguish between acute pain and chronic pain.
Chronic pain involves central sensitization, where our brain perceives a high alert of pain all the time. We need to learn how to use nervous system regulation and other strategies to down-regulate the nervous system, recognizing pain as information and shifting from a heightened sense to pain associated with a specific movement pattern. In chronic pain, there is no tissue damage at that point, whereas in acute pain, there can be tissue damage.
As always, I hope this helps you understand your neck pain a little bit more and, of course, some of the things that you can do to begin to change your pain and improve your health.
If you found this information helpful, please be sure to give it a like, share it with others, leave a comment below, and, of course, subscribe to our YouTube channel, The Movement Paradigm®, for weekly tips on mindset, nutrition, and movement.
If you’re looking for personalized guidance on your journey and feel that you need an individualized approach, please don’t hesitate to reach out to us. We would welcome the opportunity to assist you.
If you’re interested in accessing a wide range of programs, including those on nutrition, somatics, and vagus nerve exercises, as well as movement programs to help you optimize your overall wellness, consider checking out our app, The Movement Paradigm, available on both Apple and Google platforms.
Other things that might interest you: